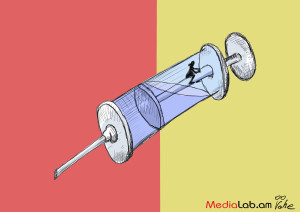
Karen (name changed at his request) who was receiving a methadone substitution treatment, living with HIV, was expelled from the program when the dose was increased to 70mg – higher than the average dose.
Methadone substitution treatment (MST) is carried out among people with opioid type dependence. Methadone is factory-made legal drug, which therapeutic dose does not cause side effects and non-adequate practices. It is taken internally (peroral) and with the help of methadone illicit drug use can be reduced or eliminated. The absence of methadone causes the recipient a severe and prolonged withdrawal.
When I was talking to Karen, it had been 3 days since he did not receive methadone; he was in an expressed withdrawal symptoms and was confused. All he wanted was going back to treatment; otherwise he would have to procure drugs and the most accessible one – “gasoline” (desomorpine).
“I take a lot of medicine. My condition gets worse with time. What shall I do? Shall I inject “gasoline”? If I inject “gasoline” after 70mg, what will I become – hobo? My teeth are rotten, if I inject “gasoline” my chin will fall apart. I have a job and I work every day. What will my colleagues say if I go to work in that condition?” says Karen.
Narcologists of Avan Narcological Clinic stopped Karen’s treatment in a result of toxic-chemical test and finding opioid drugs (apart from methadone other drugs were found).
Although Karen denies that he used other drugs, according to “Real World, Real People” NGO expert Hovhannes Madoyan the use of other is not a ground to be expelled from MST as drug addiction is a disease symptom. He compared expelling from MST to insulin deprivation for one who has diabetes and ate something sweet or to interrupting treatment for pneumonia for coughing or to not curing the tumor of a smoker because of smoking. “Doctors who do such things are sadists” says Madoyan, continuing “They took him out of the program without gradual cutting down the dose and a person will have a severe withdrawal in this case. It is not the Armenia’s narcologists who invented methadone therapy. That treatment is internationally recognized and is recommended by World Health Organization (WHO), which has a guideline on how the treatment is to be done and the guideline reads that the treatment can be stopped against the will of the patient only in cases when there is a threat to the program staff”.
In the opinion of Narcological clinic MST Project Coordinator Vache Mkrtchyan, a patient needs to be expelled from the program if they regularly continue using other drugs. He shows the point of the agreement between the patient and the clinic, which stresses that the drug user is bound to not using other drugs while on MST.
When they find out about the usage of other drugs in test for the first time, they do not expel – the program staff carry out explanatory works with the patient or they increase the dosage, assuming that maybe the low dose of methadone is becoming the reason for desire towards other drugs, but when they find a pattern on this, they take them out of the program “because the treatment that is the basis of MST – topping or reducing opioid drug abuse, is not happening. That means that it is not effective for that patient” says Mkrtchyan, mentioning that other drugs were found three times in case of Karen.
Expelling from the MST program because of using other drugs is also stated in methadone treatment guideline of Ministry of Health of the Republic of Armenia. MST has been introduced in Armenia in 2009, but the guideline was developed three years before that – in 2006. As Madoyan tells, when the guideline was being developed, no one had experience and maybe it was normal for that time: “We did not deal with these issues. It was assumed that the doctor wouldn’t come with a smile in their face and tell their patient to go and have a suffering”. The program funder Global Fund recommends following the guidelines of WHO, which is followed by western countries and where “dirty” test results are not a cause for removal.
The aim of getting tested for toxic chemicals is not to punish the patient, explains Suren Nazinyan, expert of National Institute of Health, who was once an MST coordinator as well. According to him, the purpose of taking the test is to plan the further treatment, such as dose setting or implementing psychosocial work with the patient.
“The problem is that in the whole world the main purpose of MST is not only the patient to remain free of drug use” says Nazinyan, “the global experience shows that during the past 50 years it was impossible to fully eliminate drug use among the patients with MST. The aim of MST is harm reduction, minimizing the cases of drug use, which is not only done by giving methadone, but the psychological and social worker functions are very important as well”.
The program includes a position of psychologist and there is a psychologist in the clinic, however, as Karen says, no psychologist has ever worked with him and he never saw the psychologist.
“I’ve seen a couple times a sign on the door which reads “psychologist” and days they work, but I’ve never seen who that is, what they do; I never saw the psychologist in these two years”.
Mkrtchyan says that the patient needs to apply to receive the assistance of psychologist and social worker, and Karen never did that.
It is not the patient only, who is affected by the negative consequences of being expelled from methadone program. Both Madoyan and Nazinyan stress out the consequences that can have a negative impact on both the patient and society. First of all there is a problem of transmitting infections: when the methadone recipient injects another drug then it is with a sterile syringe, but when they don’t receive methadone, the withdrawal won’t let them look for a new syringe, therefore it becomes dangerous in means of transmitting HIV or Hepatitis C.
Another problem is looking for drugs illegally. When the patient receives methadone, they won’t get engaged in theft to find another drug from the black market, because the need for other drug is not only due to suffering, but also for the desire to be in euphoric condition: “Even if they do it, they do it very very very rarely, if they have money in their hands” says Madoyan.
Mkrtchyan says that expelling from MST does not mean depriving of treatment. Another treatment – detoxification treatment was suggested, when the patient are hospitalized for 7-10 days. In order to assure the effectiveness of this treatment he brings the example of one of the patients who did not use any opium-type substances since 2009.
Nazinyan believes that detoxification treatment is not effective and the person starts using drugs after a short period of time in 95% of cases. Besides that, detoxification treatment needs to be followed by rehabilitation processes, which is not implemented in Armenia; and even if implemented, than the treatment effectiveness reaches 30% in the best case. With its effectiveness (including cost-effectiveness) significantly yields MST and this matter has been raised many times in guidelines, recommendations and other publications of international organizations working in the sphere – WHO, UN relevant departments.
When the dosage of methadone prescribed to the patient was reached 70mg, Nazinyan says, the chances are very high that detoxification treatment could not be effective: “Eliminating the methadone craving with medicine prescribed for detoxification treatment – diazepam, tramadol and antipsychotics, is not normal. Of course, a lot depends on patient’s individual features, but I am convinced that in majority of cases it makes no sense. Due to expressed morbid dependence on opium-type substances and emerging severe symptoms while having a craving, the patient will prefer to go and procure and use illegal drugs rather than try to overcome the withdrawal with diazepam”.
Karen’s unstable condition also caused him stopping antiretroviral therapy for HIV, but he preferred detoxification treatment over using drugs. On the 4th day after being expelled Karen was back to clinic and due to unbearable withdrawal and the impact of prescribed medicine, he cut his veins.
After being transferred to hospital, with the motion of Narcological clinic director Petros Semerjyan, Karen was returned to MST program, but what will happen if he uses other drugs again?
Hovhannes Ishkhanyan
Translated by Kolya Hovhannisyan